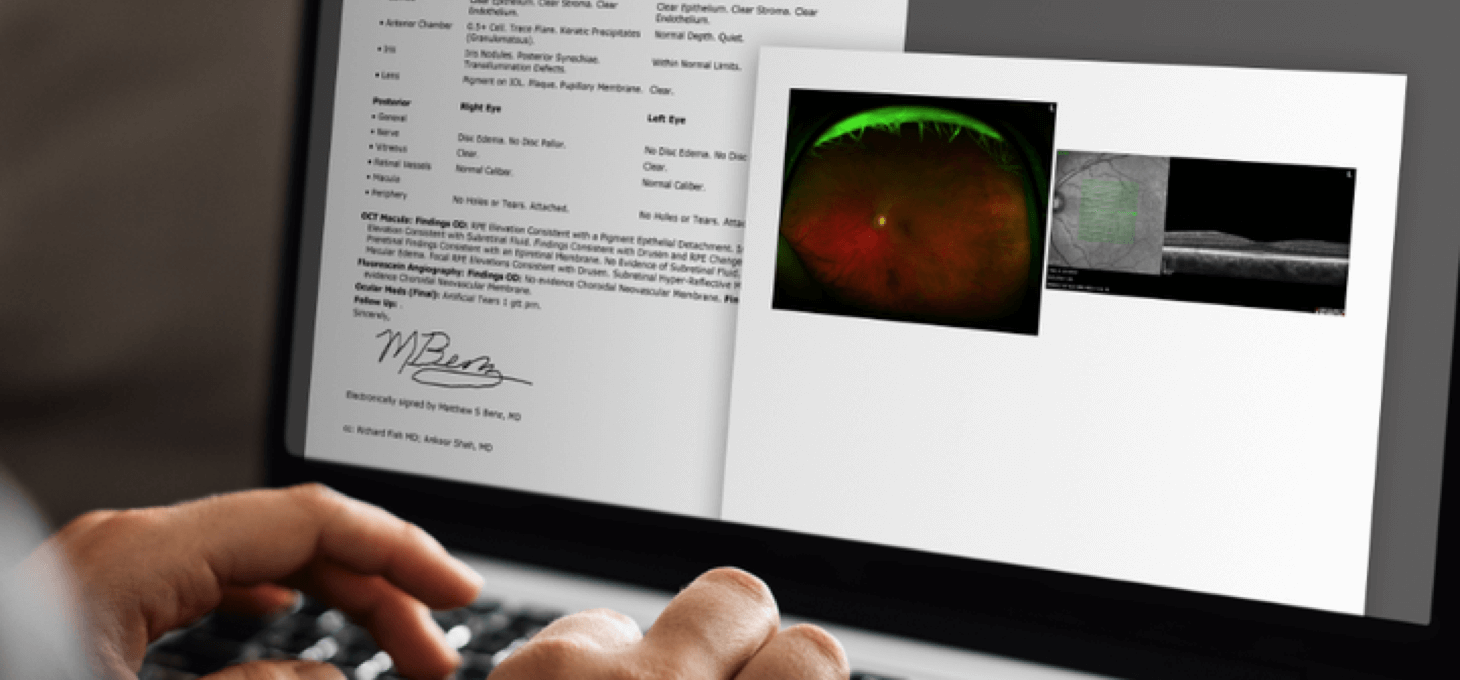
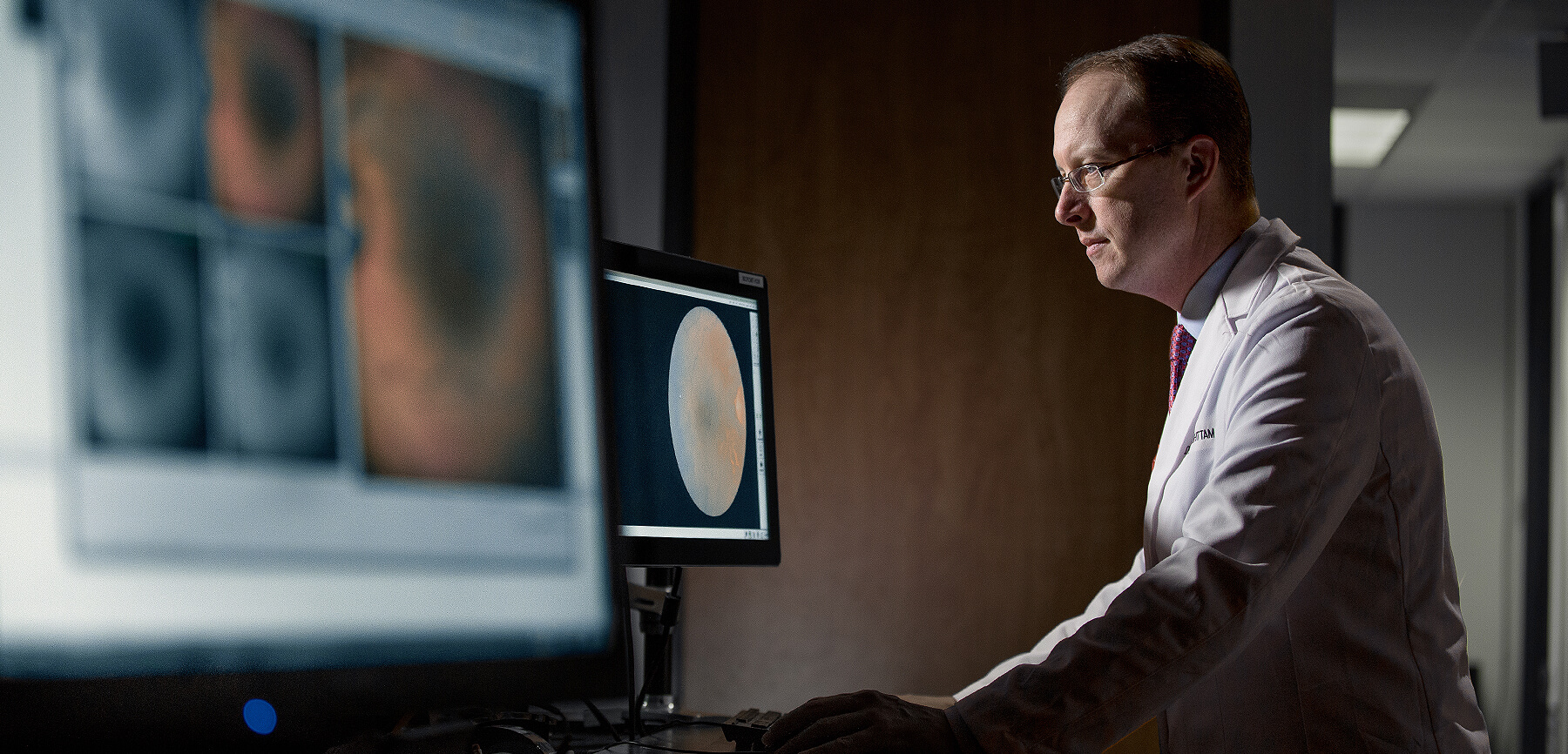
Referring doctors can now receive high quality, full color images through our HIPAA compliant RCTX Image Portal. Say goodbye to printing and faxing low-quality monochromatic images.
Retina Consultants of Texas
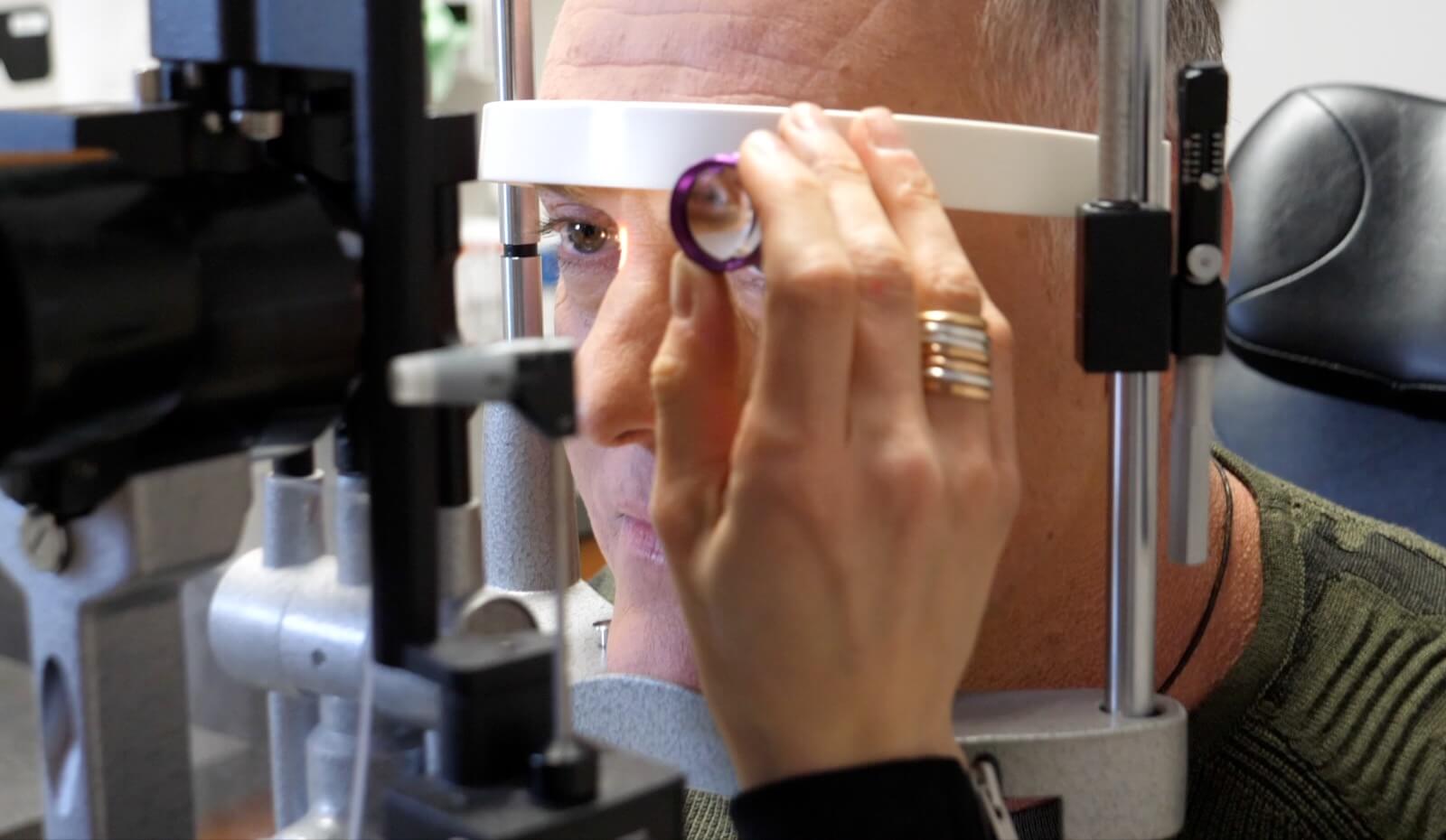
RCTX is one of the most respected retina centers in the United States. Every RCTX physician is board certified by the American Board of Ophthalmology and specializes exclusively in diseases and surgery of the retina, vitreous, and macula. Our commitment is to provide world-class expertise in the medical and surgical care of patients with retinal diseases throughout Texas and beyond while advancing science through cutting-edge research.
Memberships and Affiliations*





Getting Started: Refer a Patient
RCTX is committed to meeting your needs and exceeding your patients expectations.
Thank you for referring your patients to our care.
Referring Doctor FAQ
We understand the urgency of needing medical records and we will do our best to get them to your office as quickly as possible. Please call our office at 713-524-3434 and one of our medical records specialists will be happy to assist you.
If you have a patient that needs immediate care, please call us on your patient’s behalf at 713-524-3434 and we will get your patient scheduled right away. Please have your patient’s insurance, demographic information, and the reason for the visit available and let our call center know that your patient needs to be seen right away.
We offer three convenient ways to refer a patient to our practice. You may call us to schedule an appointment on your patient’s behalf, fax a consult request form to our office or submit your referral through our HIPAA compliant form on our website. You may also give our referral cards to your patients so they may schedule an appointment when they are ready.
You are welcome to call our office or submit a materials request through our website and we will get referral materials delivered to you.
We offer several CE events throughout the year in different parts of Southeast Texas. View our event calendar to learn more about our upcoming events.
We have 22 accessible office locations throughout Texas, all equipped to provide world-class retinal diagnostics and treatment. We invite you to learn more about our locations, here.
Attend an Upcoming CE Event
CE Events Calendar
“I have used RCTX for many years to send my patients for second opinions, evaluations, and surgery as needed for complex retinal issues. They have 100% been there for my patients regardless of their busy schedules.”Referring Optometrist
“During a routine eye examination by my optometrist it was discovered that I had torn retinas in each eye. My optometrist immediately contacted RCTX who worked me into their schedule that same day. The service I received from everyone was excellent.”L.
“Retina Consultants of Texas was recommended to me by my optometrist. She had discovered macular degeneration, and she said I must see the best. The RCTX doctor was friendly, compassionate, and VERY knowledgeable. He is a proactive, positive person, and so is his entire office. They are experts at putting a patient at ease.”P.H.
Our Retina Specialists
While preserving the vision of our patients at RCTX, our specialists stand by our commitment to you, your family, and the referring doctor to provide world-class retinal diagnostics and treatment.

Our Research
The Texas Retina Research Center (TXRRC) and The Texas Retina Research Foundation (TXRRF) provide international leadership in preventing and fighting blindness through the advancement of research in vitreoretinal diseases.
Blog and News
![RCT logo]()
New Location Alert: Vintage Park to Welcome Our 1960/Peakwood Office
July 1, 2025![]()
The Link Between Kidney Disease and Retinal Problems
June 12, 2025![]()
Inherited Retinal Diseases: How Genetic Testing Can Help
May 15, 2025![]()
Specialized Retinoblastoma Care in Texas: What Parents Should Know
April 1, 2025